Treatment
MLD is a rare disease, or “orphan” disease. There is a massive current need and this is expressed by lobbying, fundraising, agitating for research and understanding treatment.
Currently, no effective treatment is available to reverse the deterioration and loss of function that Metachromatic Leukodystrophy (MLD) causes.
At the moment, in order to get treatment for MLD, then it is essential that the sufferer is either pre-symptomatic (showing no symptoms) or in the case of Juvenile or Adult-Onset only mildly symptomatic.
Haematopoietic stem cell transplantation is available for sufferers of adult-onset MLD, but early intervention is essential to be beneficial. In the UK and the USA there are now sufferers who have had transplants who are showing little or no degeneration after 25 years.
Unrelated umbilical cord blood transplants can be used for pre-symptomatic children who have been diagnosed with Juvenile MLD.
A Clinical Trial for Gene Therapy for MLD is currently taking place in Milan, Italy. They are recruiting pre-symptomatic children with a confirmed diagnosis of Late-Infantile MLD or Juvenile MLD. It is often the case that an older sibling is diagnosed after displaying symptoms, and the younger sibling is tested prior to symptoms appearing.
A new Clinical Trial has been announced by Shire (now part of Takeda Pharmaceutical Company Ltd) for Intrathecal Enzyme Replacement Therapy for children with Late-Infantile MLD. The centre in the UK will, hopefully, be Bristol Royal Hospital for Children. Commencement will not be earlier than late 2019, and they will be recruiting children with a confirmed diagnosis of Late-Infantile MLD, who are either pre-symptomatic or symptomatic, but who have had no previous treatment such as Stem Cell Transplantation or Gene Therapy. Further details will be available later in the year.
Other possible therapies that are being researched at the moment:
- Stem cells
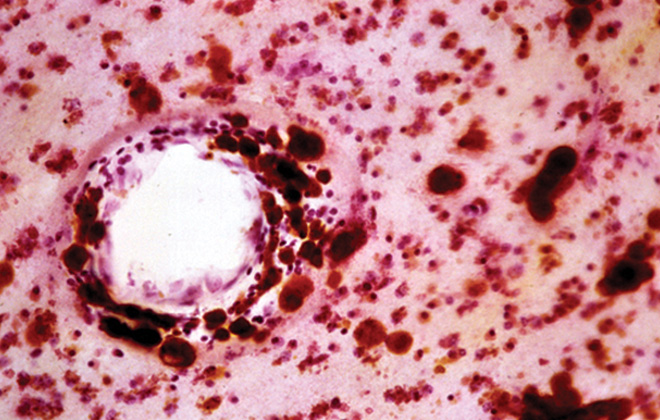
- Substrate Reduction Therapy – that is, not increasing production of the missing enzyme, but taking away the waste product produced i.e. the sulfatides which cause de-myelination
Further details of all clinical trials can be found at: clinicaltrials.gov